You’re Not Treating Acne. You’re Fueling Fungus: Why Your Skincare Could Be Making Fungal Acne Worse

If your “acne” isn’t improving or even getting worse despite every trusted product, what if the culprit isn’t bacteria at all, but yeast? Fungal acne, known medically as Malassezia folliculitis, can masquerade as regular acne, tricking you and your skincare into a cycle of ineffective routines. The scary truth? Most over-the-counter acne products don’t just fail - they can worsen your condition.
What Is Fungal Acne (and How Is It Different from Closed Comedones?)
Fungal acne is caused by an overgrowth of Malassezia yeast within hair follicles. It appears as uniform, itchy, red or skin-colored bumps, often mistaken for whiteheads or closed comedones. But there’s a critical difference:
-
Closed comedones (whiteheads) are plugged pores filled with sebum and dead skin: non-inflammatory and generally responsive to retinoids or chemical exfoliation.
-
Fungal acne, in contrast, involves yeast proliferation, often looks red, is intensely itchy, and resists traditional acne treatments.
Research shows that antifungal agents, not bacterial-targeted ingredients, are required to break the cycle of fungal breakouts. Traditional acne regimens may disrupt your skin barrier, suppress beneficial bacteria, and feed yeast, making matters worse source.
Why It Matters (Risks & Misdiagnoses)
Misidentifying fungal acne as typical acne can lead to:
-
Persistently ineffective treatments — e.g., benzoyl peroxide, salicylic acid, antibiotics.
-
Worsened symptoms — as these can disrupt the skin barrier or cause rebound yeast growth.
-
Increased irritation — antifungals like ketoconazole or zinc pyrithione may be more effective and gentler when used correctly.
For those struggling with stubborn, itchy bumps that don’t respond, fungal acne should be suspected.
How to Use or Avoid Triggers in Your Routine
Here’s a practical routine to address fungal acne effectively:
-
Introduce a gentle antifungal: Options include topical ketoconazole 2%, selenium sulfide, or zinc pyrithione. Use as directed, often 2–3 times weekly.
-
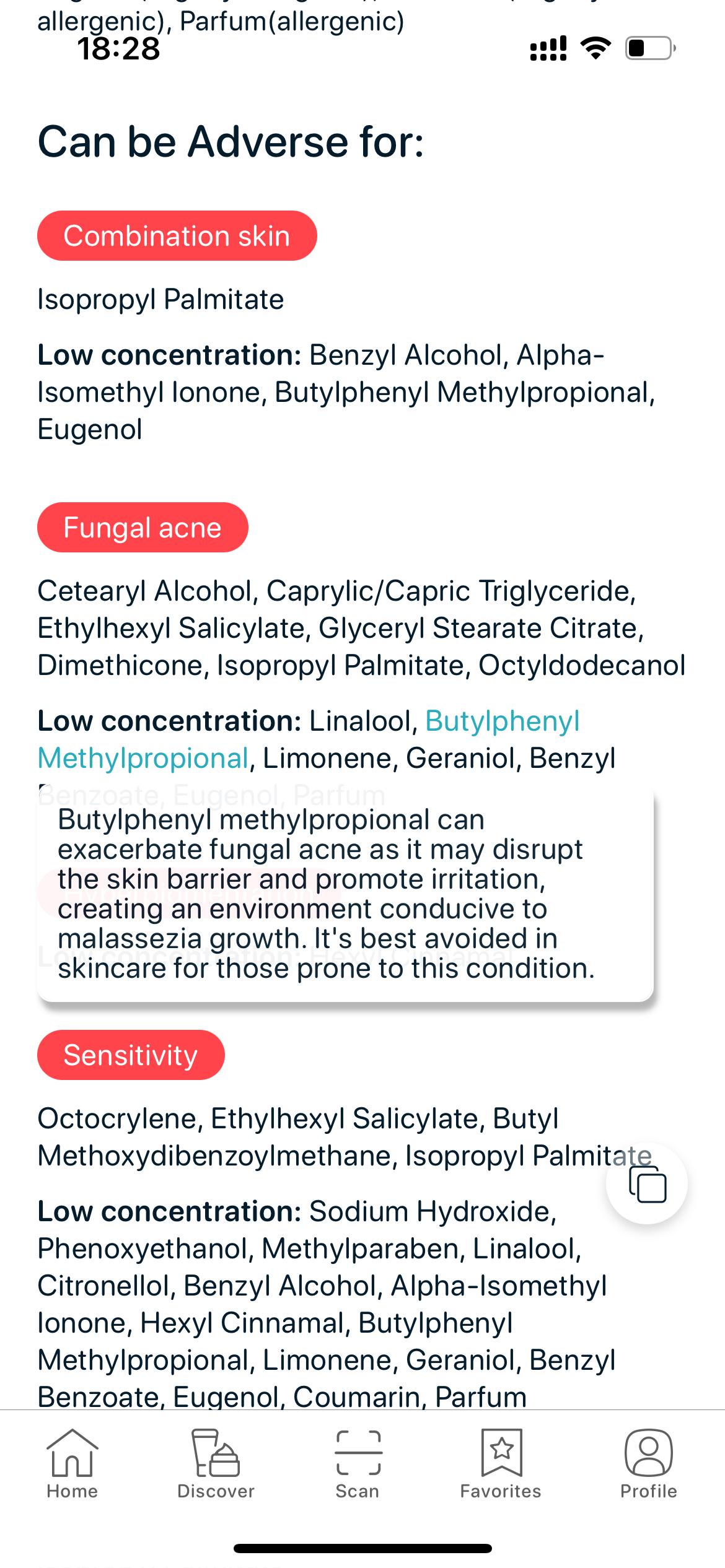
Avoid common fungal triggers: Esters (e.g., isopropyl myristate), fatty acids, polysorbates, fermented extracts, and heavy oils like cocoa butter.
-
Use barrier-supporting, non-comedogenic moisturizers: Think squalane, niacinamide, aloe vera.
-
Cleanse gently: Choose sulfate-free, low-pH cleansers.
-
Introduce exfoliants carefully: Avoid over-exfoliating the skin, which can impair your barrier.
-
Apply sunscreen daily: Antifungal products can increase sun sensitivity.
How SkinBuddy Helps You Manage Fungal Acne
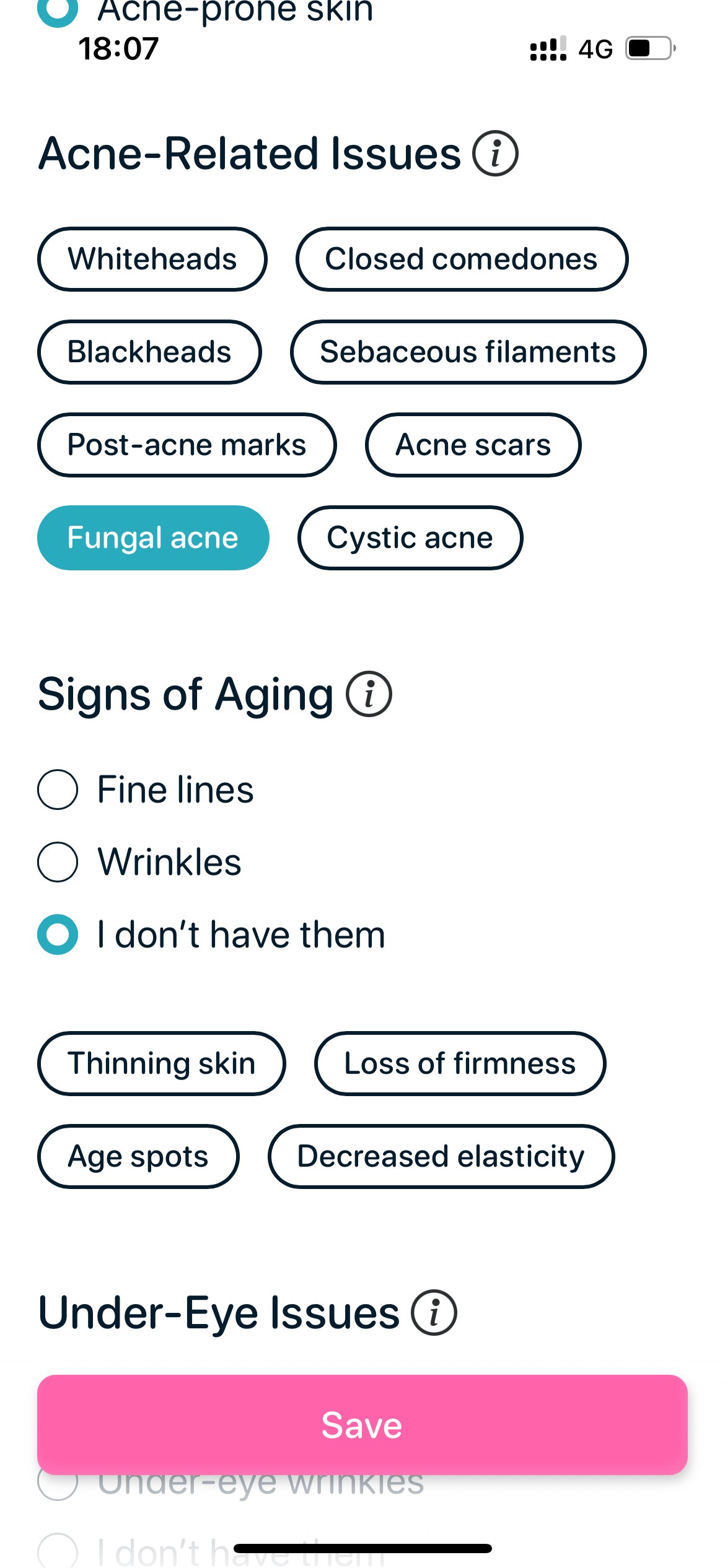
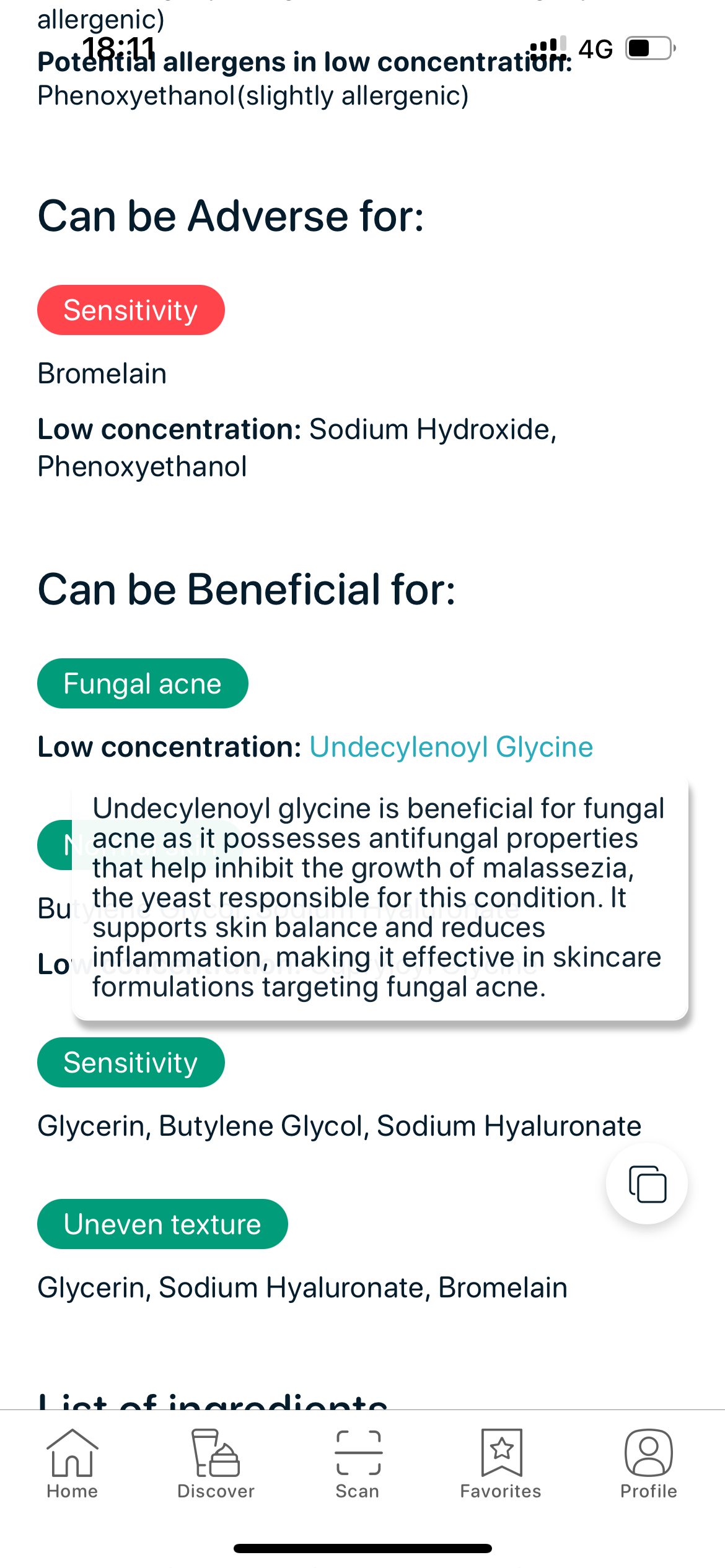
In SkinBuddy, you can choose “Fungal Acne” in your skin profile:
- Every product you scan will instantly show ingredients that are beneficial, neutral, or harmful for fungal acne
- Detailed ingredient-level explanations are included so you understand why each ingredient is flagged
- In “Discover Ideal Match,” you’ll get fungal acne–safe recommendations based on your other skin goals (hydration, redness, etc.)
Try SkinBuddy to find out what works for your skin, and what doesn’t.
Scan your skincare, avoid pore-clogging or irritating ingredients, and discover smarter product matches. Open the web app or download the mobile app to get started.
or
Check Products OnlineCheck if your skincare suits your skin type, sensitivity, or acne-prone needs at skinbuddy.app and discover better options that match your routine and goals. SkinBuddy makes it easy, fast, and science-backed.
Scan to get started:

Web App (mobile only)

App Store & Google Play
FAQs About Fungal Acne & Ingredients
-
Can fungal acne be confused with regular acne?
Yes. Fungal acne often looks like small, itchy bumps and doesn’t respond to typical acne treatments. -
What ingredients should I avoid?
Esters, polysorbates, fermented extracts, and certain oils may feed yeast. -
Are mineral oil and silicones bad?
They're not fungal-feeding, but they can trap other pore-clogging ingredients. -
Can I use retinoids or exfoliants?
Yes, but gently. They can irritate the skin if your barrier is compromised. -
Can fungal acne come back?
Yes, especially if your skincare or environment promotes yeast overgrowth. Ongoing maintenance is key.
Final Thoughts
It’s not just acne, it might be fungal acne, and that changes everything. From stubborn breakouts to itchiness that won’t quit, identifying the right cause is crucial for effective treatment. With SkinBuddy, you’ll never have to guess. Our ingredient intelligence flags every product for you, so you can calm your skin, fast
Ready to say goodbye to fungal acne?
Download the SkinBuddy app and get product suggestions tailored to your fungal acne–safe routine.